Frozen Shoulder
Frozen shoulder is also called adhesive capsulitis and causes pain and stiffness in the shoulder. Over time, the shoulder becomes very hard to move both actively and passively.
Frozen shoulder is usually a self-limiting disease meaning after a period of worsening symptoms, frozen shoulder tends to get better, although full recovery may take up to 18 months to 3 years. Physical therapy, with a focus on shoulder flexibility, is the primary treatment recommendation for frozen shoulder.
Frozen shoulder most commonly affects people between the ages of 40 and 60, and occurs in women more often than men. In addition, people with diabetes are at an increased risk for developing frozen shoulder.
Description
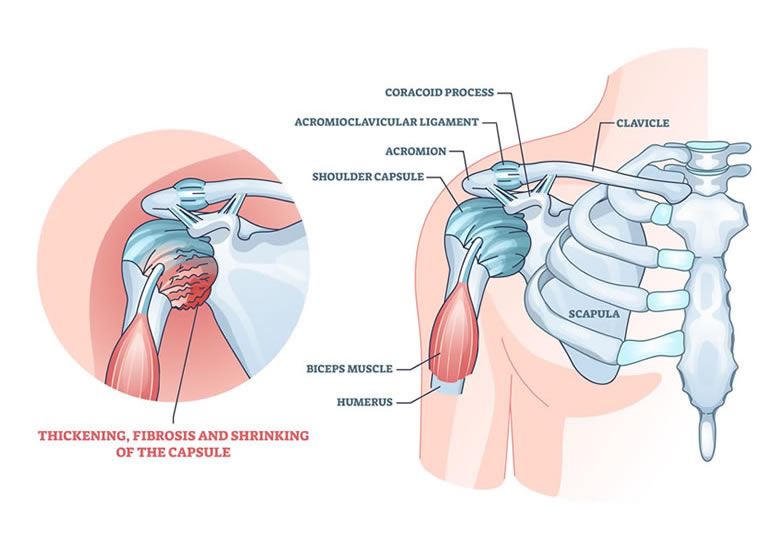
In frozen shoulder, the shoulder capsule which is essentially the covering of the shoulder thickens and becomes stiff and tight. Thick bands of tissue — called adhesions — develop. In many cases, there is less synovial fluid in the joint. The most common cause of frozen shoulder is idiopathic meaning no specific cause is responsible for developing the same. More often than not there is microtrauma to the shoulder in a diabetic which does not heal, thereby starting an inflammatory cascade and leading up to the development of frozen shoulder. In more than 50 percent cases there is a chance that this frozen shoulder will affect the opposite shoulder within 3 years of affection of the primary shoulder.
The hallmark signs of this condition are severe pain and being unable to move your shoulder -- either on your own or with the help of someone else. It develops in three stages:
- Stage 1: Freezing
In the "freezing" stage, you slowly have more and more pain. As the pain worsens, your shoulder loses range of motion. Freezing typically lasts from 6 weeks to 9 months. - Stage 2: Frozen
Painful symptoms may actually improve during this stage, but the stiffness remains. During the 4 to 6 months of the "Frozen" stage, daily activities may be very difficult. - Stage 3: Thawing
Shoulder motion slowly improves during the "Thawing" stage. Complete return to normal or close to normal strength and motion typically takes from 6 months to 2 years.
Diagnosis & Tests
How is frozen shoulder diagnosed?
To diagnose frozen shoulder, doctor will:
- Discuss your symptoms and review your medical history.
- Conduct a physical exam of your arms and shoulders:
- The doctor will move your shoulder in all directions to check the range of motion and if there is pain with movement. This type of exam, in which your doctor is moving your arm and not you, is called determining your “Passive Range of Motion.”
- The doctor will also watch you move your shoulder to see your “Active Range of Motion.”
- The two types of motion are compared. People with frozen shoulder have limited range of both active and passive motion.
- X-rays of the shoulder are also routinely obtained to make sure the cause of the symptoms is not due to another problem with the shoulder such as calcification or rotator cuff pathology or arthritis. Advanced imaging tests, such as magnetic resonance imaging (MRI) and ultrasound, are usually not needed to diagnose frozen shoulder. They may be taken to look for other problems, such as a rotator cuff tear.
Management & Treatment
What are the treatments for Frozen Shoulder?
Treatment usually involves pain relief methods until the initial phase passes. If the problem persists, therapy and surgery may be needed to regain motion if it doesn’t return on its own.
Some simple treatments include:
- Cold Compresses: These help reduce pain and swelling.
- Medicines that Reduce Pain & Swelling: These include nonsteroidal anti-inflammatory drugs (NSAIDs). Other painkiller/anti-inflammatory drugs may be prescribed by your doctor.
- Physical Therapy Stretching and range of motion exercises taught by a Physical Therapist.
- Injections: More severe pain and swelling may be managed by steroid injections. A corticosteroid, such as cortisone, is injected directly into the shoulder joint. The pre-requisite for this is that the sugar levels if diabetic should be under control.
- Home Exercise Program: Continue exercise program at home.
- Manipulation Under Anesthesia: During this surgery, you will be put to sleep and your doctor will force movement of your shoulder. This will cause the joint capsule to stretch or tear to loosen the tightness. This will lead to an increase in the range of motion.
- Shoulder Arthroscopy: Your doctor will cut through the tight parts of your joint capsule (capsular release). Small pencil-sized instruments are inserted through small cuts around your shoulder.
If these simple treatments have not relieved pain and shoulder stiffness after about a year trial, other procedures may be tried. These include:
These two procedures are often used together to get better results.
Prevention
Can frozen shoulder be prevented?
The chance of a frozen shoulder can be prevented or at least lessened if physical therapy is started shortly after any shoulder injury in which shoulder movement is painful or difficult. Avoiding trauma to the shoulder and keeping your HbA1c levels under control forms the mainstay of prevention of developing frozen shoulder.
To know more kindly contact the best orthopaedic surgeon Dr. Rahul Modi for further queries.
This surgery is frequently performed by the best orthopaedic surgeon Dr. Rahul Modi for treating Frozen Shoulder.