Recurrent Shoulder Dislocation
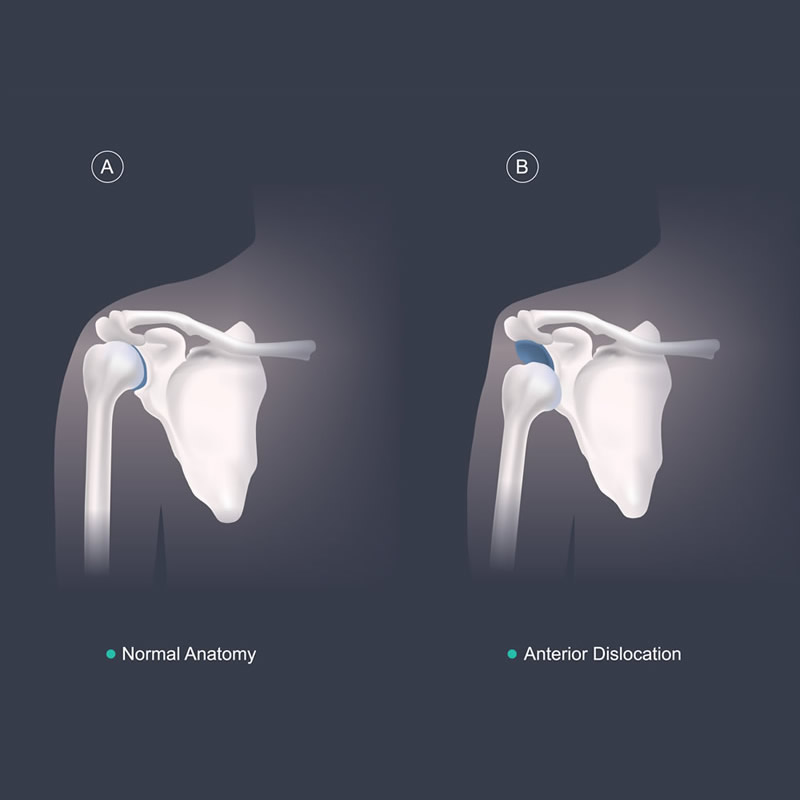
Shoulder joint is vulnerable for dislocation more often than any other joint in the body. The extreme mobility it enjoys jeopardizes its stability.
Ninety-five percent of the shoulder dislocation is anterior and the remaining five percent is posterior.
The anatomy of the shoulder joint can be compared to a golf ball on a tee or a lemon on a spoon wherein the spoon is smaller and the lemon is bigger, thus making it a highly unstable joint. To stabilize this further the cup of the shoulder joint which is known as the glenoid on which the ball that is the head of the humerus rests is covered on all sides with specialized tissue which is called as the labrum. This labrum serves 2 primary purposes. One it increases the surface area of the cup holding the ball making it more stable and second it has a vacuum like effect which holds the ball in place in its entire range of motion. The first time there is a shoulder dislocation there is a tear in the anteroinferior part of this labrum thereby making the shoulder prone to recurrent dislocation. The disruption between the Anterior Inferior Labrum and the glenoid, as seen in traumatic anterior instability, was termed the “Essential Lesion” by bankart in 1938. Subsequently it has been dubbed the “Bankart Lesion.”
Treatment
Anterior dislocation of the shoulder is an emergency and has to be immediately reduced. There are various methods of reduction but the most commonly used method is the kocher’s method. The various steps of this method of reduction are under general anesthesia, longitudinal traction is applied along the line of the humerus, external rotation of the arm, adduction and internal rotation of the arm.
After Treatment
After the reduction, the arm is usually fastened to the chest with a body bandage or a universal shoulder immobilizer for a minimum period of two to three weeks. Recurrence occurs due to the damage to the tissues or the bone during the first or subsequent dislocations. The force required to dislocate a shoulder in the 2nd, 3rd and 4th dislocations is lesser than the first. Left untreated, the damage increases and the shoulder starts dislocating in normal day to day activities or in sleep.
Recurrent Anterior Dislocation of the Shoulder (RDS)
This is a very common complication of anterior dislocation of shoulder and accounts for greater than 80 percent of dislocations of the upper extremity.
Age at the time of initial dislocation is an important prognostic factor, recurrence rate being 55 percent in patients 12 to 22 years old, 37 percent in 23 to 29 years old, and 12 percent in 30 to 40 years old.
Causes
- Size and nature of damage at the time of initial dislocation.
- Greater the trauma, more the incidence.
- Younger the patient, more is the recurrence.
Mechanism of Dislocation
In some individuals, the dislocation can be predictable and can be avoided. In others, the mechanism is unpredictable and thus makes it a very disabling problem. The usual mechanism of dislocation is external rotation in abducted position.
Pathological Anatomy
No single deformity is responsible for recurrent dislocation of shoulder. Three important reasons have been cited.
Triad of recurrent dislocation
- Bankart’s Lesion (Essential Lesion)
- Hill-Sachs Lesion
- Erosion of anterior rim of glenoid cavity
Clinical Features
The patient gives history of a previous episode of traumatic dislocation. After that, there could be one or two instances of repeated dislocations during abduction. The clinical features and the presentation will be like in anterior dislocation of shoulder but the far less severity. There could be wasting of deltoid, supraspinatus and infraspinatus muscles.
Clinical Tests
Three tests help to identify instability of the shoulder prone to develop RDS:
- The Sulcus Test
- The Apprehension Test
- Relocation Test
Investigations
- Radiology: A study of the plain x-ray of the shoulder helps detect the various lesions described above.
- CT Scan: Helps to analyze the defects of rds more clearly.
- MRI: This helps to evaluate the entire spectrum of the problem in recurrent shoulder dislocation namely the bony, soft tissue and labral defects that cannot be identified by the x-rays. This helps to plan the treatment better.
Treatment
There is no role of conservative treatment in Recurrent Dislocation of Shoulder.
The patient is advised to avoid abduction and external rotation of the shoulder. However, surgery is the treatment of choice and is indicated if the patient has more than three episodes of RDS.
Multiple surgerical options are available to prevent recurrent dislocation. Few are mentioned here. All the surgeries aim at correction of the essential lesions and prevent external rotation of the arm.
- Bankart’s Operation +/- Remplissage
- Latarjet Surgery
- Putti-platt’s Operation
- Eden Hybinette
- Bristow’s
- Mclaughlin’s
Inferior Dislocation (Luxatio Erecta)
Here the head of the humerus is below the glenoid cavity and the humeral shaft is pointing overhead. It is due to hyperabduction force and is a rare injury. Here shoulder is locked in 100 to 160° of abduction with the forearm behind the head.
To know more kindly contact the best orthopaedic surgeon Dr. Rahul Modi for further queries.
This surgery is frequently performed by the best orthopaedic surgeon Dr. Rahul Modi for treating Recurrent Shoulder Dislocation.