Recurrent Patellar Dislocation
Recurrent Patellar instability is a phenomenon in which the patient suffers from multiple patellar dislocations, subluxations or a sense of instability.
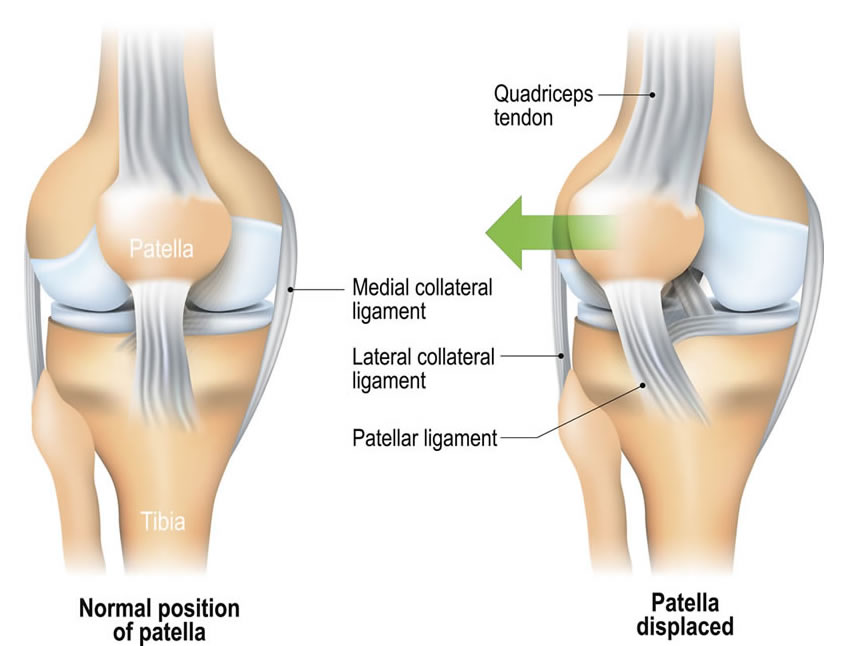
The dislocations are almost always directed towards the outer side, and there is a clear history of an episode of instability (described as a deformity of the knee) followed by reduction either spontaneously or after manipulation.
Epidemiology
Acute traumatic patellar dislocation (first time) is the most common injury around the knee in a growing child that is before the age of 18 years. In a few cases recurrent patellar dislocation can also occur in a slightly older child till the age of 25 years. Very rarely adults beyond the age of 25 are affected. The younger the child at the time of the first dislocation, more the chances of recurrent dislocation.
Studies show that if the first dislocation occurs below the age of 15 years, the chances of second dislocation in the same knee is more than 50%.
Risk factors associated with recurrent dislocations
- Young age [children and adolescents] at the time of initial dislocation
- Female gender
- Dysplasia of the patellofemoral joint
- Family history
- Generalized ligamentous laxity — benign hypermobility syndrome
- Syndromic — Down’s Syndrome, Rubinstein-taybi Syndrome, Nail Patella Syndrome
Pathological Mechanisms
- Geometry of patellofemoral articulation and congruency
- Consequences of limb malalignment
- Soft tissue restraints
Clinical Presentation
History of the knee giving away or more specifically the “Knee Cap” giving away or moving outwards should arouse the suspicion of possible patellar instability. The initial episode is almost always following a traumatic fall especially while playing.
This is followed by sensation of instability with or without pain and may be aggravated during certain day to day activities like getting up from a sitting position, coming down the stairs or while pivoting, as one may do while abruptly making a sharp turn outward. The second and subsequent dislocations might be traumatic but lesser force is required to dislocate the patella.
The location of the pain is variable and may be either anteriorly or medially.
Physical examination includes generalized hypermobility or ligamentous laxity by appropriate systemic evaluation (beighton hypermobility score).
Local examination may reveal swelling, parapatellar tenderness and an effusion.
In the subacute or chronic scenario, these signs are usually not present.
Patellar maltracking is evident during the range of the motion in a few cases.
Radiographic Evaluation
The three main modalities of imaging relevant to evaluation of patellofemoral instability are plain radiographs, ct and mri. Sometimes a standing full length scanogram is required for checking the alignment. All of these are complementary to each other and are used to detect four main abnormalities, which constitute a risk towards developing instability namely, trochlear dysplasia, patella alta, increased tt-tg offset and patellar tilt.
Treatment
Non Operative Treatment
Non Operative Treatment is the initial treatment modality, which involves symptomatic treatment in the form of rest, analgesics and ice immediately following an episode of dislocation.
Aspiration of any hemarthrosis that is present following an acute episode of dislocation has been shown to be helpful in the speedier recovery.
Prolonged splintage or immobilization has not shown to be of any benefit and may increase the risk of stiffness and quadriceps wasting. Subsequently the mainstay of treatment would be physiotherapy with or without a trial of taping.
Physiotherapy involves closed chain exercises for the knee along with targeted strengthening exercises for vastus medialis obliquus.
Operative Treatment
There are numerous surgical procedures described for patellar instability, and this is indicative of the fact that there is no single surgical solution to this multifactorial problem.
Operative treatment is considered only when nonoperative measures have failed and there is persistence of symptomatic instability causing functional impairment.
Surgical interventions can be divided into bony and soft tissue procedures and depending on the anatomical level of intervention, they can be further classified into proximal, intra articular and distal procedures.
Proximal
- Soft Tissue — MPFL Reconstruction / Extra-Articular lateral release / medial soft tissue plication or advancement
- Bony — Femoral Osteotomies — To correct rotational / angular malalignment
Intra - Articular
- Soft Tissue - Arthroscopic Lateral Release
- Bony — Trochleoplasty
Distal
- Soft Tissue - Patellar Ligament Realignment
- Bony — Tibial Tubercle Osteotomy
To know more kindly contact the best orthopaedic surgeon Dr. Rahul Modi for further queries.
This surgery is frequently performed by the best orthopaedic surgeon Dr. Rahul Modi for treating Recurrent Patellar Dislocation.