Osteoarthritis of the Knee
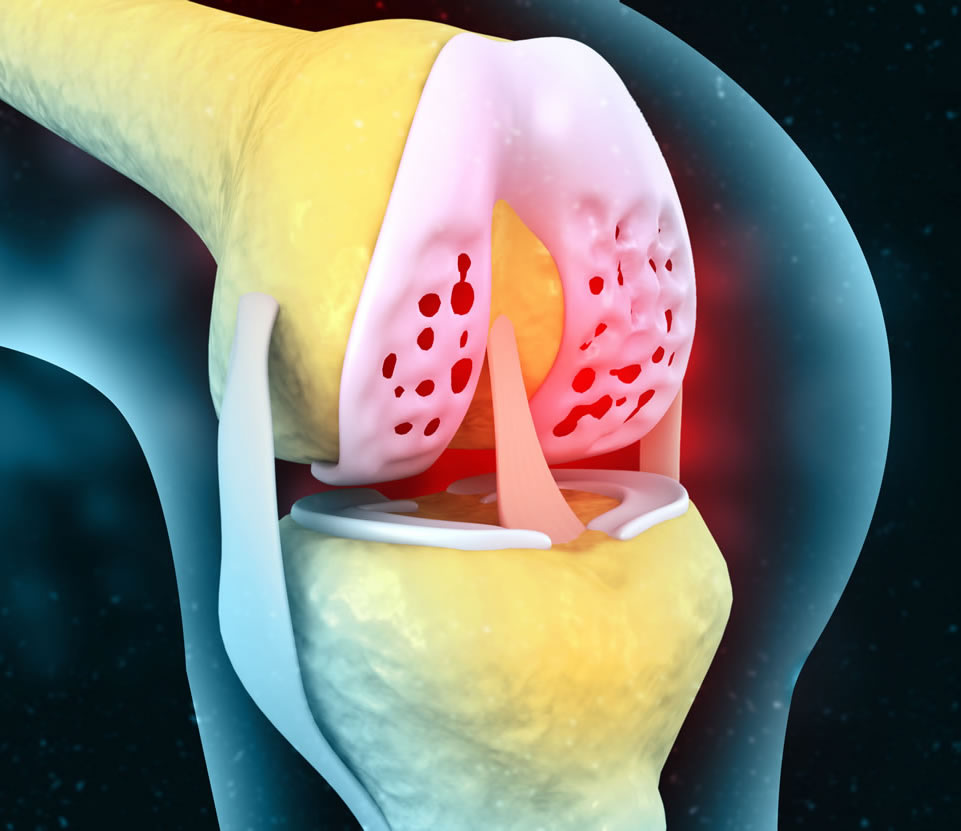
It is defined as a degenerative, non-inflammatory joint disease characterized by destruction of articular cartilage and formation of new bone at the joint surfaces and margins.
It could be primary or secondary and the former is more common.
Osteoarthritis affects the synovial joints, though it can affect any joint, it is most common in the knee as it is a weight bearing joint.
Primary osteoarthritis of the knee
There is a multifactorial etiology playing a part in the development of osteoarthritis — obesity, genetics and heredity, occupation involving prolonged standing, sports, multiple endocrinal disorders and multiple metabolic disorders, anatomical alignment of an individual all contribute to the development of osteoarthritis.
Clinical features:
- Predominant symptom is pain which decreases on walking.
- The pain is poorly localized and is dull aching in nature.
- The patient has mild swelling of the knee joint and complains of early morning stiffness.
- The swelling is most often at the back of the knee which is called the bakers cyst.
- Minimal tenderness localized to the inner aspect of the knee and cracking sound on movement called crepitus can be elicited.
- If there are loose bodies in a joint, the patient gives history of locking or giving way.
- Terminal movements of the knee are restricted.
- Bow leg like deformity which is called genu varum deformity may be seen in very advanced cases.
- Minimal fluid in the knee which is called effusion may be present.
Investigations
1. Laboratory investigations are usually within normal limits.
2. Xray of the knee joint in standing position is the most important diagnostic tool. The following are the radiological features seen in osteoarthritis of the knee:
- Loss of joint space (due to destruction of articular cartilage).
- Sclerosis (due to increased cellularity and bone deposition).
- Subchondral cysts (due to synovial fluid intrusion into the bone).
- Osteophytes (due to revascularization of remaining cartilage and capsular traction)
- Bony collapse (due to compression of weakened bone).
- Loose bodies (due to fragmentation of osteochondral surface).
- Deformity and malalignment (due to destruction of capsules and ligaments).
Other Investigations
- Arthroscopic examination: this allows direct inspection and visualization of the damaged joint surfaces. But arthroscopy alone for diagnostic purposes is rarely used. This is used only in conjunction with a mri which shows meniscal tears or loose bodies which is the cause of the acute pain and arthroscopy is a tool which can give pain relief in a minimally invasive manner by treating only the acute cause of the pain. Hence arthroscopy is not only diagnostic but also therapeutic.
- Synovial fluid analysis shows non-inflammatory picture.
Treatment
Conservative Methods
Non Pharmacological Treatment
This is the initial and main stay of treatment in oa knees. The important recommendations of arc are:
- Self education — Educating the patient and his relatives measures about the disease is the most important aspect of the non-pharmacological treatment and should be done first. Activity modification becomes the most important treatment in a patient of osteoarthritis in the early stages. This can help to reduce the rate of progression significantly thereby increasing pain free surgery free knee life.
- Health Professional Social Support
- Weight Loss
- Physiotherapy
- Therapeutic Exercises
- Assistive Devices
- Occupational Therapy
- Aerobic Exercise Program
- Strengthening of the Quadriceps
- Supervised Fitness Walking Program
- Swimming / Hydrotherapy
- Modifications of activity of daily living
Mechanical Aids
- Cane in the contralateral hand
- Mechanical Aids
- Shoe Inserts
- Shoe Supplements - Good shock absorber, good mediolateral support, adequate arch support, calcaneal cushion.
- Lateral Heel Wedges - To reduce pain of Medial Tibiofemoral Joint QA.
- Knee brace and support in varus knees.
- Medial taping of the patella in pf diseases
- Lightweight knee braces in tf diseases.
Physiotherapy
Physical modalities that may contribute to pain relief include the application of cold (cold packs or ice packs).
Pharmacologic Drugs:
Appropriate drugs with injection therapy if needed will be suggested by the orthopedic doctor.
Alternative Therapies
- Acupuncture
- Biofeedback
- Naturopathy
- Aquatic Physical Therapy
- Massage
- Acupressure
- Tai Chi
- Balneotherapy
- Yoga
Intra-articular Injections
Intra articular injections play a very important part of the management of osteoarthritis. These work as temporary measures to relieve pain without undergoing surgery. There are 3 different injections which we may inject in the knee.
- Steroid – very potent as far as pain relief is concerned. Cheapest of all the 3 alternatives. But has maximum side effects and needs to be used with caution in diabetics.
- PRP (Platelet Rich Plasma) – As is autologous has least or no side effects. Pain relief is mild to moderate.
- Hyaluronic Acid (Viscosupplementation) – It most closely resembles the knee joint fluid and has anti-inflammatory properties too which help in pain relief. It is the costliest alternative.
Surgery
Surgical methods can be broadly classified into 2 main groups.
Joint Preservation Knee Surgeries
Joint preservation surgeries include
1. Arthroscopy
Arthroscopy of the knee in a case of osteoarthritis is indicated in the following situations – acute traumatic + degenerative meniscal tears, loose bodies in the knee causing locking, synovectomy with arthroscopic debridement to postpone knee replacement by a finite period of time.
2. High Tibial Osteotomy
This is done in the young arthritic knees with bow legs alignment (varus). This shifts the weight bearing axis of the limb from the medial compartment to the centre of the knee thereby offloading the medial compartment of the knee and thereby reducing pain. It is sometimes used in conjunction with arthroscopic procedures.
3. Cartilage Resurfacing Surgeries
These surgeries are limited to focal cartilage lesions causing accelerated wear and tear. These include procedures like autologous chondrocyte implantation (aci) and osteochondral autologous transfer system (oats).
Joint Replacement Knee Surgeries
1. Partial Knee Replacement (Unicondylar Knee Replacement)
Partial knee replacament is used when only one part of the knee is damaged (mostly the medial) and the other compartments (lateral and patellofemoral) have not undergone degeneration.
2. Total Knee Replacement
Total knee replacement in mumbai is also known as total knee arthroplasty. Total knee replacement in mumbai can help relieve pain and restore function in severely diseased knee joints. The procedure involves cutting away damaged bone and cartilage from your thighbone, shinbone and kneecap and replacing it with an artificial joint (prosthesis) made of metal alloys, high-grade plastics and polymers. We have the best total knee replacement surgeons operating and giving best results. From improved mobility and independence to increased confidence and a heightened quality of life, total knee replacement is a life-changing surgery. You're finally free from pain and stiffness you can now do the things you love to do, from hiking to dancing. With a new knee joint, you'll have the freedom to enjoy life in ways that were once unimaginable. A new knee means better sleep, improved mobility, and a happier outlook on every day. You deserve this chance at happiness.
To know more kindly contact the best orthopaedic surgeon Dr. Rahul Modi for further queries.
This surgery is frequently performed by the best orthopaedic surgeon Dr. Rahul Modi for treating Knee Arthritis.